The vagus nerve is a complex and fascinating part of the human body. It plays a critical role in regulating various bodily functions, including digestion, heart rate, and even mood. In recent years, researchers have been uncovering its potential impact on the cervical spine – the part of our spine that extends from the base of the skull to the upper back. This article aims to explore the intricate relationship between the vagus nerve and the cervical spine and shed light on the potential implications for our overall health and well-being.
Understanding the Vagus Nerve
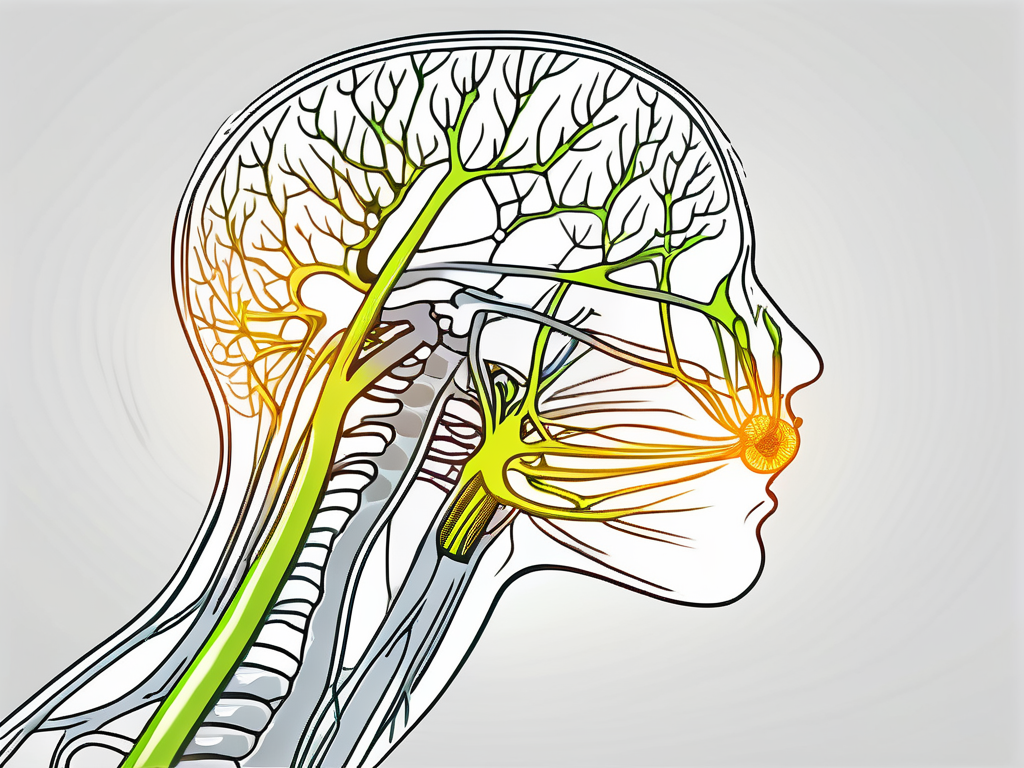
Before delving into its relationship with the cervical spine, it is essential to understand the vagus nerve and its role in the body. Named after the Latin word for “wandering,” the vagus nerve is the longest cranial nerve and is essential for regulating various bodily functions. It originates in the brainstem and extends down through the neck, chest, and abdomen, connecting many vital organs along the way.
The vagus nerve consists of multiple branches that supply different organs and tissues throughout the body. It carries important sensory and motor signals between the brain and various organs, such as the heart, lungs, stomach, and intestines. This communication allows the body to maintain homeostasis and adapt to changes in the environment.
One of the main branches of the vagus nerve, known as the recurrent laryngeal nerve, plays a crucial role in controlling the muscles responsible for vocalization. Without the vagus nerve, our ability to speak and produce sound would be severely impaired.
In addition to its role in regulating bodily functions, the vagus nerve also plays a significant role in our emotional well-being. It is often referred to as the “wandering nerve” because it sends branches to various areas of the body, including the heart and gut, which are closely linked to our emotions. This connection explains why we often experience physical sensations in our stomach or heart when we feel strong emotions, such as fear or excitement.
Furthermore, the vagus nerve is closely intertwined with the enteric nervous system, often referred to as the “second brain.” This complex network of neurons is located in the walls of the digestive system and is responsible for regulating digestion, nutrient absorption, and gut motility. The vagus nerve acts as a vital link between the brain and the enteric nervous system, allowing for seamless communication and coordination.
Anatomy and Function of the Vagus Nerve
The vagus nerve consists of multiple branches that supply different organs and tissues throughout the body. It carries important sensory and motor signals between the brain and various organs, such as the heart, lungs, stomach, and intestines. This communication allows the body to maintain homeostasis and adapt to changes in the environment.
One of the primary functions of the vagus nerve is to regulate heart rate and blood pressure. It achieves this by sending signals to the heart, instructing it to beat at an appropriate rate and strength. Additionally, the vagus nerve helps to reduce inflammation in the body, which is crucial for maintaining overall health and preventing chronic diseases.
The vagus nerve also plays a crucial role in digestion. It stimulates the production of stomach acid and digestive enzymes, which are necessary for breaking down food and absorbing nutrients. Furthermore, the vagus nerve helps to regulate gut motility, ensuring that food moves through the digestive system at an appropriate pace.
In addition to its role in regulating bodily functions, the vagus nerve is also involved in various cognitive processes. It has been linked to memory formation and retrieval, attention, and emotional regulation. Studies have shown that stimulating the vagus nerve can improve cognitive performance and enhance mood.
The Vagus Nerve and the Nervous System
As part of the parasympathetic nervous system, the vagus nerve primarily functions to counterbalance the “fight or flight” response of the sympathetic nervous system. It promotes calming and restorative processes, helping to regulate heart rate, reduce inflammation, and enhance digestive functions.
When activated, the vagus nerve triggers the release of acetylcholine, a neurotransmitter that promotes relaxation and inhibits stress responses. This activation leads to a decrease in heart rate, blood pressure, and respiratory rate, allowing the body to conserve energy and recover from stressors.
Furthermore, the vagus nerve plays a crucial role in the body’s immune response. It helps to regulate inflammation by releasing anti-inflammatory cytokines and inhibiting the production of pro-inflammatory molecules. This immune-modulating effect is essential for maintaining a healthy immune system and preventing chronic inflammation.
Overall, the vagus nerve is a vital component of the nervous system, involved in regulating numerous bodily functions and maintaining overall health. Understanding its anatomy and function is crucial for comprehending its relationship with the cervical spine and its potential impact on our well-being.
The Cervical Spine and its Relationship with the Vagus Nerve
The cervical spine, comprising the first seven vertebrae in the spine, plays a crucial role in supporting the head, protecting the spinal cord, and facilitating movement. Its intricate relationship with the vagus nerve has been a subject of growing interest among researchers.
Anatomy of the Cervical Spine
The cervical spine consists of seven vertebrae, often referred to as C1 to C7, with intervertebral discs between them for cushioning and flexibility. Each cervical vertebra has unique characteristics that contribute to the overall function of the spine.
The uppermost vertebra, C1 or the atlas, is a ring-shaped bone that supports the skull. It allows for the nodding motion of the head, enabling us to say “yes.” The C2 vertebra, known as the axis, has a unique structure that allows for the rotation of the head, enabling us to say “no.” These two vertebrae work together to provide a wide range of motion for the head and neck.
The remaining cervical vertebrae, C3 to C7, are responsible for providing stability and support to the neck. They are larger and stronger than the upper two vertebrae, as they bear the weight of the head and help maintain proper alignment.
How the Vagus Nerve Interacts with the Cervical Spine
The vagus nerve, also known as the tenth cranial nerve, has several direct and indirect anatomical connections with the cervical spine. It passes through the neck, alongside the spinal column, and is in close proximity to the cervical vertebrae and associated muscles.
Research suggests that the vagus nerve’s close relationship with the cervical spine could potentially impact its function and health. The vagus nerve is responsible for regulating various bodily functions, including heart rate, digestion, and inflammation. Any disruption or dysfunction in the vagus nerve can have widespread effects on the body.
Various factors, such as misalignment or compression of the cervical vertebrae, could potentially affect the vagus nerve. Structural abnormalities or conditions like cervical radiculopathy or cervical spondylosis might exert pressure on the vagus nerve, potentially leading to complications or dysfunction.
Moreover, the muscles surrounding the cervical spine also play a role in the interaction between the vagus nerve and the cervical spine. Tension or tightness in these muscles can affect the nerve’s function, further emphasizing the importance of maintaining a healthy cervical spine.
Understanding the intricate relationship between the cervical spine and the vagus nerve is crucial for healthcare professionals in diagnosing and treating various conditions. By addressing any issues in the cervical spine, such as misalignments or muscle imbalances, healthcare providers can potentially improve vagus nerve function and overall well-being.
The Vagus Nerve’s Influence on Cervical Spine Health
The bidirectional relationship between the vagus nerve and the cervical spine opens up intriguing possibilities regarding their influence on each other’s health and well-being. Understanding this relationship can provide valuable insights into potential therapeutic approaches and treatment options.
The vagus nerve, also known as the “wandering nerve,” is the longest cranial nerve in the body. It originates in the brainstem and extends down to various organs, including the heart, lungs, and gastrointestinal tract. Along its journey, the vagus nerve interacts with the cervical spine, which consists of seven vertebrae and supports the head and neck.
Research suggests that the vagus nerve plays a crucial role in regulating various bodily functions, such as heart rate, digestion, and inflammation. It also has an impact on mental health, as it is involved in the regulation of mood and stress responses. Given its extensive reach and influence, it is not surprising that the vagus nerve’s health can affect the well-being of the cervical spine and vice versa.
Vagus Nerve Stimulation and its Effects on the Cervical Spine
Vagus nerve stimulation (VNS) is a therapeutic technique that involves delivering mild electrical impulses to the vagus nerve. It has shown promise in the management of various conditions, including epilepsy, depression, and even migraines. While VNS primarily targets the vagus nerve, its effects on the surrounding cervical spine may also be significant.
By stimulating the vagus nerve, VNS has the potential to enhance the function and blood flow to the cervical spine. This increased blood flow could promote tissue healing and alleviate symptoms associated with cervical spine conditions. Additionally, VNS may help modulate pain signals in the cervical spine, providing relief to individuals suffering from chronic neck pain.
Furthermore, VNS has been found to have anti-inflammatory effects, which could benefit individuals with inflammatory conditions affecting the cervical spine, such as rheumatoid arthritis or cervical spondylosis. The precise mechanisms through which VNS influences the cervical spine are still being investigated, but the potential therapeutic applications are promising.
However, further research is needed to explore the specific effects of VNS on the cervical spine. Clinical trials and studies focusing on the interaction between VNS and cervical spine health will help elucidate the underlying mechanisms and determine the optimal parameters for stimulation.
Potential Risks and Complications
As with any medical intervention, vagus nerve stimulation is not without its risks and potential complications. It is crucial to consult with a healthcare professional to determine the suitability of VNS for individual cases and to understand the potential risks involved. Each person’s unique health profile and medical history must be considered before embarking on any intervention.
Some of the potential risks associated with VNS include infection at the implantation site, voice changes, cough, shortness of breath, and hoarseness. These complications are relatively rare but should be discussed with a healthcare provider to make an informed decision.
Additionally, VNS may interact with certain medications or medical conditions, making it important to disclose all relevant information to the healthcare professional. They can assess the potential risks and benefits of VNS and determine if it is a suitable treatment option for the individual.
In conclusion, the relationship between the vagus nerve and the cervical spine is complex and multifaceted. Vagus nerve stimulation holds promise as a therapeutic approach for various conditions, including those affecting the cervical spine. However, further research is needed to fully understand the mechanisms and potential benefits of VNS on cervical spine health. Consulting with a healthcare professional is crucial to determine the suitability of VNS and to weigh the potential risks and benefits for each individual.
Therapeutic Approaches Involving the Vagus Nerve and Cervical Spine
When it comes to therapeutic techniques involving the vagus nerve and cervical spine, there is a wide range of options available. While vagus nerve stimulation is a prominent approach, there are also various non-invasive and surgical interventions that can potentially impact these areas and provide relief for individuals suffering from related conditions.
Non-Invasive Techniques for Vagus Nerve Stimulation
One of the non-invasive techniques gaining attention is transcutaneous vagus nerve stimulation (tVNS). This approach involves applying mild electrical impulses to the skin overlying the vagus nerve. By doing so, the goal is to modulate the activity of the vagus nerve without the need for invasive procedures.
tVNS is still being extensively researched, but early findings show promise as a potential treatment option for conditions related to the vagus nerve and cervical spine. It is believed that by stimulating the vagus nerve non-invasively, it may be possible to alleviate symptoms and improve overall well-being in individuals suffering from various disorders.
Studies have shown that tVNS can have positive effects on conditions such as chronic pain, depression, anxiety, and even epilepsy. By targeting the vagus nerve, which plays a crucial role in regulating bodily functions and maintaining homeostasis, non-invasive stimulation techniques like tVNS offer a novel approach to managing these conditions.
Surgical Interventions and the Vagus Nerve
While non-invasive techniques like tVNS show promise, there are cases where surgical interventions may be necessary to address specific cervical spine or vagus nerve conditions. These interventions aim to alleviate symptoms and improve the overall quality of life for individuals facing more severe or complex issues.
One such surgical procedure is spinal decompression surgery, which involves relieving pressure on the spinal cord or nerves in the cervical spine. This procedure can be beneficial for individuals suffering from conditions like herniated discs, spinal stenosis, or other spinal abnormalities that may be compressing the vagus nerve or causing related symptoms.
Another surgical intervention that may be considered is vagus nerve repair. This procedure aims to restore the function of the vagus nerve by repairing any damage or addressing any underlying issues that may be affecting its proper functioning. Vagus nerve repair can be a complex procedure that requires the expertise of a skilled surgeon and careful evaluation of the potential benefits and risks involved.
It is important to note that surgical interventions come with their own set of considerations and risks. Before making any decisions, it is crucial to consult with a medical professional who specializes in the treatment of vagus nerve and cervical spine conditions. They will be able to thoroughly evaluate your specific case, discuss the potential benefits and risks, and guide you towards the most appropriate treatment approach.
In conclusion, therapeutic approaches involving the vagus nerve and cervical spine encompass a wide range of options. From non-invasive techniques like tVNS to surgical interventions such as spinal decompression surgery or vagus nerve repair, there are various ways to address conditions related to these areas. The key is to work closely with a medical professional to determine the most suitable approach for your specific needs, ensuring the best possible outcome for your overall well-being.
Future Research Directions in Vagus Nerve and Cervical Spine Interaction
The understanding of the intricacies of the vagus nerve and cervical spine relationship is still evolving. Ongoing research efforts are exploring emerging trends and potential future directions to further unravel the mysteries surrounding this intriguing connection.
One area of future research interest lies in understanding the role of the vagus nerve in regulating inflammation within the cervical spine. Inflammation is a key factor in many cervical spine conditions, such as cervical radiculopathy and cervical spondylosis. By elucidating the mechanisms by which the vagus nerve modulates inflammation, researchers hope to develop targeted interventions that can alleviate pain and improve functional outcomes for patients.
Another promising avenue for future research is investigating the impact of vagus nerve stimulation on the autonomic nervous system. The autonomic nervous system plays a crucial role in regulating various bodily functions, including heart rate, blood pressure, and digestion. By understanding how vagus nerve stimulation affects autonomic function, researchers can potentially develop novel therapies for conditions such as autonomic dysregulation and dysautonomia.
Emerging Trends in Vagus Nerve Research
Recent studies have highlighted the potential therapeutic applications of vagus nerve stimulation beyond its direct impact on specific conditions. Researchers are investigating the potential benefits of VNS in promoting general well-being, enhancing cognitive function, and even mitigating the effects of neurodegenerative diseases. These emerging trends hold significant promise for the future of healthcare.
One emerging trend in vagus nerve research is the exploration of its role in mental health disorders. Studies have shown that vagus nerve stimulation may have a positive impact on conditions such as depression, anxiety, and post-traumatic stress disorder. By further investigating the underlying mechanisms and optimizing stimulation protocols, researchers aim to develop more targeted and effective treatments for these debilitating mental health conditions.
Another exciting area of research is the potential use of vagus nerve stimulation in enhancing memory and cognitive function. Preliminary studies have shown promising results, suggesting that VNS may improve memory consolidation and retrieval. This research has implications not only for individuals with cognitive impairments but also for healthy individuals looking to optimize their cognitive performance.
The Future of Cervical Spine Treatment
As our understanding of the vagus nerve and cervical spine interaction deepens, it is likely to have a profound impact on how we approach the treatment of conditions affecting the cervical spine. Research exploring the potential benefits of therapies targeting the vagus nerve is imperative to pave the way for more effective and personalized treatments in the future.
One area of future development in cervical spine treatment is the integration of neuromodulation techniques. By combining vagus nerve stimulation with other modalities, such as spinal cord stimulation or transcutaneous electrical nerve stimulation, researchers hope to achieve synergistic effects that can provide enhanced pain relief and functional improvement for patients with cervical spine disorders.
Furthermore, the advent of bioengineering and regenerative medicine holds promise for the future of cervical spine treatment. Researchers are exploring the use of tissue engineering approaches to develop biocompatible scaffolds that can promote tissue regeneration and repair in the cervical spine. By harnessing the regenerative potential of stem cells and incorporating them into these scaffolds, it may be possible to restore function and alleviate symptoms in patients with cervical spine injuries or degenerative conditions.
In conclusion, the impact of the vagus nerve on the cervical spine is a complex and intriguing area of research. While much remains to be discovered, it is evident that this relationship holds significant implications for our overall health and well-being. If you suspect any issues with your cervical spine or experience symptoms related to the vagus nerve, it is crucial to consult with a medical professional for a comprehensive evaluation and appropriate guidance.
As you’ve delved into the fascinating world of the vagus nerve and its profound impact on the cervical spine, you’re likely eager to learn more about this vital component of your well-being. The “My Vagus Nerve & Me Book” is a treasure trove of knowledge, offering a deep dive into the vagus nerve’s functions, from regulating your heart rate and digestion to its role in mental health and beyond. Discover the secrets of stimulating this powerful nerve both naturally and artificially, and unlock the potential to enhance your immune system, support liver detoxification, and much more. Don’t miss this opportunity to explore one of the most advanced systems within your body. Get My Vagus Nerve & Me eBook today and embark on a journey to optimal health and well-being.